A solitary pulmonary nodule (SPN) or coin lesion is a mass in the lung smaller than 3 centimeters in diameter. It can be an incidental finding found in up to 0.2% of chest X-rays and around 1% of CT scans.
The nodule most commonly represents a benign tumor such as a granuloma or hamartoma, but in around 20% of cases it represents a malignant cancer, especially in older adults and smokers. Conversely, 10 to 20% of patients with lung cancer are diagnosed in this way. If the patient has a history of smoking or the nodule is growing the possibility of cancer may need to be excluded through further radiological studies and interventions, possibly including surgical resection. The prognosis depends on the underlying condition.
Video Solitary pulmonary nodule
Definition
Nodular density is used to distinguish larger lung tumors, smaller infiltrates or masses with other accompanying characteristics. An often used formal radiological definition is the following: a single lesion in the lung completely surrounded by lung parenchyma (functional tissue) with a diameter less than 3 cm and without associated pneumonia, atelectasis (lung collapse) or lymphadenopathies (swollen lymph nodes).
Maps Solitary pulmonary nodule
Cause
Not every round spot on a radiological image is a solitary pulmonary nodule: it should not be confused with the projection of a structure of the chest wall or skin, such as a nipple, a healing rib fracture or electrocardiographic monitoring.
The most important cause to exclude is a form of lung cancer, including rare forms such as primary pulmonary lymphoma, carcinoid tumor and a solitary metastasis to the lung (common unrecognised primary tumor sites are melanomas, sarcomas or testicular cancer). Benign tumors in the lung include hamartomas and chondromas.
The most common benign coin lesion is a granuloma (inflammatory nodule), for example due to tuberculosis or a fungal infection, such as Coccidioidomycosis. Other infectious causes include a pulmonary abscess, pneumonia (including Pneumocystis carinii pneumonia) or rarely nocardial infection or worm infection (such as dirofilariasis or dog heartworm infestation). Lung nodules can also occur in immune disorders, such as rheumatoid arthritis or granulomatosis with polyangiitis, or organizing pneumonia.
An SPN can be found to be an arteriovenous malformation, a hematoma or an infarction zone. It may also be caused by bronchial atresia, sequestration, an inhaled foreign body or pleural plaque.
Diagnosis
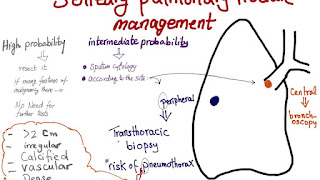
Diagnosis can be made by a lung biopsy. Small biopsies obtained by core needle or bronchoscopy are commonly used for diagnosis of lung nodules. CT guided percutaneous transthoracic needle biopsies have also proven to be very helpful in the diagnosis of SPN. Several features help to distinguish benign conditions from possible lung cancer. The first parameter is the size of the lesion: the smaller, the less risk for malignant cancer. Benign causes tend to have a well defined border, whereas lobulated lesions or those with an irregular margin extending into the neighbouring tissue tend to be malignant.
Growth of nodules also helps determine their status (malignant, infectious, or benign) in the body which is based on the time it takes for the volume to double. The typical values are less than 20 days, less than 100 days, or more than 400 days for infection based, malignant, and benign nodules respectively.
If there is a central cavity, then a thin wall points to a benign cause whereas a thick wall is associated with malignancy (especially 4 mm or less versus 16 mm or more). In lung cancer, cavitation can represent central tumor necrosis (tissue death) or secondary abscess formation. If the walls of an airway are visible (air bronchogram), bronchioloalveolar carcinoma is a possibility.
An SPN often contains calcifications. Certain patterns of calcification are reassuring, such as the popcorn-like appearance of hamartoma. An SPN with a density below 15 Hounsfield units on computed tomography tends to be benign, whereas malignant tumors often measure more than 20 Hounsfield units. Fatty tissue inside hamartomas will have a strongly negative value on the Hounsfield scale.
The growth velocity of a lesion is also informative: very fast or very slow growing tumors are rarely malignant, in contrary to inflammatory or congenital conditions. It is therefore important to retrieve previous imaging studies to see if a lesion was presented and how fast its volume is increasing. This is more difficult for nodules smaller than 1 centimeter. Moreover, the predictive value of stable lesion over a period of 2 years has been found to be rather low and unreliable.
Prevention and screening
The medical history, physical examination and imaging results form the basis of the initial risk assessment and determine the further course of action. Most patients will have a CT scan.
Several patient factors may influence the likelihood of a benign versus a malignant condition: these include previous exposure to smoke or other carcinogens such as asbestos and previously diagnosed cancer, respiratory infections, or Chronic obstructive pulmonary disease. A patient with airway symptoms, especially coughing up blood (hemoptysis), is more likely to have cancer compared to a patient with no respiratory symptoms.
Treatment
When a solitary pulmonary nodule is identified, plans for further action are made based on the likelihood that the nodule could be malignant cancer. If the risk of malignancy is thought to be low, follow-up imaging (usually serial CT scans) can be planned at a later time. If the initial impression is that there is a high likelihood of cancer, then a surgical intervention (such as the Video-assisted thoracoscopic surgery) is appropriate (provided that the patient is fit for surgery). For cases in which some action is required but the situation is uncertain, guidelines exist to recommend how much surveillance there should be in defined circumstances. If a pulmonary nodule has not grown for two years and the person has no prior history of cancer then that nodule is extremely unlikely to be malignant. If the nodule is "ground glass" then longer follow up is required but the same applies. More frequent CT scans than what is recommended has not been shown to improve outcomes but will increase radiation exposure and the unnecessary health care can be expected to make the patient anxious and uncertain.
If there is an intermediate risk of malignancy, further imaging with positron emission tomography (PET scan) is appropriate (if available). Around 95% of patients with a malignant nodule will have an abnormal PET scan, while around 78% of patients with a benign nodule will look normal on PET (this is the test sensitivity and specificity). Thus, an abnormal PET scan will reliably pick up cancer, but several other types of nodules (inflammatory or infectious, for example) will also show up on a PET scan. If the nodule has a diameter below 1 centimeter, PET scans are often avoided because there is an increased risk of falsely normal results. Cancerous lesions usually have a high metabolism on PET, as demonstrated by their high uptake of FDG (a radioactive sugar). If the lesion is found on further imaging to be suspicious, it should be surgically excised (via thoracotomy or video-assisted thoracic surgery) to confirm the diagnosis by microscopical examination.
In selected cases, nodules can also be sampled through the airways using bronchoscopy or through the chest wall using needle aspiration (which can be done under CT guidance). Needle aspiration can only retrieve groups of cells for cytology and not a tissue cylinder or biopsy, precluding evaluation of the tissue architecture. Theoretically, this makes the diagnosis of benign conditions more difficult, although rates higher than 90% have been reported. Complications of the latter technique include hemorrhage into the lung and air leak in the pleural space between the lung and the chest wall (pneumothorax). However, not all these cases of pneumothorax need treatment with a chest tube.
Other imaging techniques include PET-CT (simultaneous PET scan and CT scan with superposition of the images), magnetic resonance imaging (MRI) or single photon emission computed tomography (SPECT).
Footnotes
Source of the article : Wikipedia